The first question that was submitted today was what are the key symptoms I might expect to see in a patient with PNH, and does the patient always present with hemoglobinuria?
 |
| References: Jalbert JJ, et al. Blood. 2019;134(Suppl 1):3407.; Rachidi S, Musallam KM, Taher AT. Eur J Intern Med. 2010;21(4):260-267. |
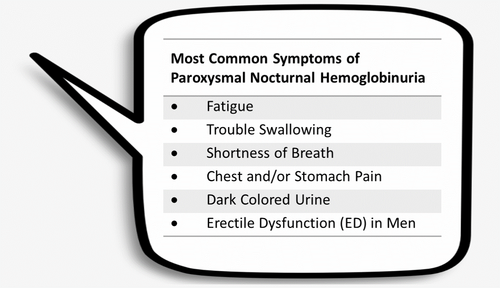
In my experience, patients with PNH very often just complain of profound fatigue, clinically, these patients can be mildly anemic. Usually, they will have something low in the CBC. Usually, its anemia, but they might also have low platelets or a low white cell count. In general, people with PNH have some form of an aplastic anemia on the background. In my experience, sometimes they have myelodysplastic syndrome. That's relatively rare, but it does occur. In patients where I'm entertaining the possibility of a PNH diagnosis, usual features are history of thrombotic events, elevated LDH, and fatigue as I mentioned before.
People sometimes complain of Coca-Cola-colored urine, especially in the morning, but that's actually not a cardinal feature of the disease in my experience. Sometimes they can complain of paroxysms, that's why paroxysmal, in association with stress events. That might not occur at all. If the patient has a PNH clone, but they were undergoing chronic hemolysis, their red cell clone might be quite small. That's one of the reasons why PNH flow cytometry testing tests three different lineages. Red cells, are reported as type one, type two, or type three. Type three PNH cells would be those that are completely missing GPI anchor proteins.
Then they usually will do testing using FLARE, fluorescent lysine, or other markers for granulocytes and for monocytes. If you see a patient who has a clone of granulocytes or monocytes that is larger, say greater than 10% or greater than 15% or 20%, but a red cell clone that's relatively small, that suggests that the patient has hemolyzed their red cell clone. If you were to give that patient a complement inhibitor that patient might normalize their red cell clone size, and that red cell hemolysis may be actually mediating the anemia that you're observing.
The second question I have here is, “In a patient with PNH who had a history of thrombosis, is indefinite anticoagulation always required, or the standard of care?” I think historically the answer was once the patient thrombosed, keeping them on an anticoagulant lifelong was necessary. I think the data is really changing in the sense that anti-C5 inhibitor therapy has proven to be very effective at preventing breakthrough thrombotic events in people with PNH.
If you have a patient who has a history of a thrombosis, and that thrombosis has been treated with anticoagulation and the patient's thrombotic area has cleared up, and they're no longer symptomatic, in that patient who is on long-standing anti-complement inhibitor therapy and whose hemolysis is well controlled, I would consider discontinuing anticoagulation. I do have some patients in my practice where they have had recurrent thrombotic events, and once they've had more than one, or they have sequelae of thrombosis, I usually do not stop anticoagulation.
I think that's a case-by-case basis, but in the case where you have a single thrombotic event in a single location, the patient is completely resolved in terms of their symptoms. It might not be unreasonable to consider discontinuation of anticoagulation.
The third question we have is, “How far are we from having an oral agent available for PNH?” I think we have several agents that are currently in clinical development.
- BCX9930 for the Treatment of PNH in Subjects Not Receiving Other Complement Inhibitor Therapy (REDEEM-2)
- Study of Efficacy and Safety of Twice Daily Oral Iptacopan (LNP023) in Adult PNH Patients Who Are Naive to Complement Inhibitor Therapy (APPOINT-PNH)
- Study of Danicopan in Participants With Paroxysmal Nocturnal Hemoglobinuria (PNH)
One of them is currently being reviewed. I think the answer is probably within a year out from having an oral agent. A couple of agents are really, as we described in the talk are pretty far. There were some hold-ups in some of those studies, but I think those are now back online. I think the answer is relatively soon and probably within the next year.
